A Parent’s Survival Guide to Biomedical Therapies in ASD
To enlarge this document for easy viewing please click Fullscreen below.
A Parent’s Survival Guide to Biomedical Therapies in Autism Spectrum Disorders
Gregory Brown MD
I.
Getting Started
A.
Read, read, read
1. 2.
Books (see Appendix M) Websites
a)
Autism Research Institute (ARI)
(1)
www.autism.com/index.htm
b)
TACA - Talk About Curing Autism
(1)
www.talkaboutcuringautism.org/index.htm
c)
Autism One
(1)
www.autismone.org/
3.
Electronic Newsletters
a)
Autism Research Institute
(1)
www.autism.com/ari/newsletter/subscribe.htm
b)
Schafer Autism Report
(1)
www.sarnet.org/
c)
Many others exist, usually focused on specific topics.
(1)
“Chelating Kids” is an example.
1
(a)
http://health.groups.yahoo.com/group/Chelat ingKids2/
4. 5.
Conference tapes Video and audio webcasts
a)
“Defeat Autism Now!” conference webcasts
(1)
www.danwebcast.com/
b)
Autism TV
(1)
www.up-to-date.com/autism.tv/index.html
c)
Autism One Radio
(1)
http://autismone.org/radio/
B.
Develop your support structure
1. 2. 3. 4.
Relatives Friends Therapists Biomedical Support Groups
a) b)
Live Online
II.
Reclaiming your child’s health
A.
What you can do before your see a biomedical practitioner
1.
Organize
a)
Gather copies of all your child’s medical records and
(1) (2)
Organize them chronologically Organize test results separately
2
(3)
Get vaccine lot #’s from pediatric records
(a)
http://medalerts.org/vaersdb/hotlot.html to see if your child’s vaccines came from known “hotlots”.
b)
Write a short (1-2 page) chronologic history of your child so you don’t have to repeat the basics to every practitioner. Include:
(1) (2)
Major illnesses and behavioral responses Regressions (major and minor) and any suspected causes Major life events
(3) c)
Write a short treatment history. Include:
(1)
Type and name (if available) of treatment
(a) (b) (c) (d)
Psychiatric pharmaceuticals Antibiotics Biomedical interventions Educational interventions
(2) (3)
Dates or child’s age at time of treatment Brief description of response
(a) (b) (c)
Positive Negative Neutral
d)
Videotape your child and add to it periodically.
3
e)
File a VAERS (Vaccine Adverse Event Reporting System) report if you think vaccines contributed to your child’s autism.
(1) (2)
http://vaers.hhs.gov/ This one of the most effective methods we have of getting the message of “vaccine injury” to the policy makers!
2.
Diet
a)
Food – A child’s worst enemy or best friend
(1)
Digestion and absorption – Getting nutrition from food Food Allergies – Immune activation by food Food Neurology – Neurotransmitter mimicry by food
(2) (3)
b)
Cleaning up your family’s diet
(1) (2)
Become a label reader!!! If it has more than three syllables or you can’t pronounce it, it probably doesn’t belong in your child’s mouth.
c)
Starting a “Specific” diet
(1)
Why start a diet
(a)
Gastro-Intestinal (GI) healing
(i) (ii) (iii)
Maldigestion Leaky gut Dysbiosis
4
(b)
Food “Neurology”
(i)
Peptide molecules mimicking chemical neurotransmitters
(a)
Gluten and casein acting like endorphin molecules
(ii)
Food additives mimicking excitatory neurotransmitters
(a) (b) (c) (d)
Artificial food dyes Monosodium Glutamate Nitrates and nitrites Natural phenols and salicylates
(2)
Choosing a diet
(a)
Any diet should be a clean diet!
(i) (ii)
As organic as possible Free of preservatives, artificial colorings, artificial flavorings and artificial sweeteners.
(b)
Anything your child craves is probably bad for them. GF/CF is a good place to begin.
(i)
(c)
Greatest response for your effort.
(3)
“Preparing to begin”
(a)
See Appendix A
(4)
Avoid common pitfalls to GF/CF
(a)
Research the diet first.
5
(i)
Familiarize yourself with all of gluten’s and casein’s aliases . www.gfcfdiet.com Practice label reading.
(ii) (iii) (b)
Enlist the cooperation (even grudging cooperation) of all those who are feeding your child. Remove casein and gluten separately.
(i) (ii) (iii)
(c)
Remove casein first. Remove gluten two weeks later. Don’t “wean” them off.
(a)
“Cold Turkey” will maximize your chances of recognizing a positive response.
(iv) (v)
Limit sugar, soy and corn. Limit carbohydrates.
(a)
Don’t try to replace all gluten carbs with gluten-free carbs. Simple sugars and simple starch feed yeast and clostridia.
(b)
(d)
Remove gluten and casein completely.
(i)
Infractions are sabotage early in the diet. Infractions may be planned later in the diet.
(ii)
(e)
Be prepared for withdrawal.
6
(i)
Behavior will likely get worse before it gets better. It is not “normal” to have behavior changes, bad or good, when a food is removed.
(a)
(ii)
These are direct evidence of undesirable effects of these foods on the body.
(f)
Keep both gluten and casein out for at least three months.
(i)
This is necessary to see the benefits of the removed “neurologic” effects. Food allergy benefits may take much longer.
(ii)
(g)
These are healing diets!
(i) (ii)
They are not lifelong diets. You will probably need to address dysbiosis, yeast, heavy metals and digestion as well as diet before GI healing can be achieved.
(5)
Dealing with the picky eater
(a) (b)
www.nourishinghope.com www.gfcf-diet.talkaboutcuringautism. org/picky-kids-eating-autism.htm Persevere! The vast majority of kids will eat when their bodies relearn what hunger is.
(c)
(6)
When and how to stop a diet
7
(a)
Stopping when you think it hasn’t helped
(i)
Reintroduce gluten & casein separately. Do it in a big way!
(ii) (b)
Stopping when it helped but you think it’s been long enough
(i) (ii)
Reintroducing casein (Appendix K) Reintroducing gluten (Appendix L)
3.
Beginning supplements (Appendix C)
a)
What supplements can I begin on my own?
(1) (2)
Melatonin (if having sleep issues) Probiotics
(a)
See Appendix E
(3) (4) (5) (6) (7) (8) (9) b)
Magnesium (Mg) Zinc (Zn) Essential Fatty Acids Multivitamin (MVI) Vitamin C B Vitamins Digestive enzymes
How do I get supplements into my child?
(1)
Most supplements are available in a variety of forms.
8
(a)
Capsules (which can be opened and mixed with foods or liquids) Tablets (can be crushed and mixed) Powders Liquids Chewables (multivitamins, enzymes, CoQ10) Puddings (fish oil)
(b) (c) (d) (e)
(f) (2)
Minerals can be added when you cook. (Mg, Zn, Calcium) Fruit juice or fruit smoothies can hide many tastes. See Appendix G for further suggestions.
(3) (4) 4.
Priorities
a)
Gastro-intestinal
(1)
Constipation
(a)
See Appendix D
(2)
Food addictions
(a) (b) (c)
Gluten, Casein Simple sugars, Simple starches Excitotoxins
(i)
See Appendix B
(3)
Yeast
(a) (b)
See Appendix H Probiotics
9
(i) (c) (d)
See Appendix E
Natural Antifungals Activated Charcoal
(i)
See Appendix F
b)
Pain
(1) (2)
Many “autistic behaviors” are responses to pain! Ibuprofen can be very useful both in diagnosing “pain behavior” and in treating that pain.
B.
Working with your child’s Primary Medical Doctor (PMD)
1.
If your child’s PMD thinks you’re crazy, it’s time for a new PMD. If they’re cooperative, some lab tests can be helpful.
a) b) c) d)
2.
Complete Blood Count (CBC) Comprehensive Metabolic Panel (CMP) Serum Ferritin and Iron Panel Celiac Panel (prior to starting Gluten Free diet)
(1)
Inability to obtain this test is not a reason to not start the diet.
e) f)
Thyroid Stimulating Hormone (TSH) Venous Lead
(1)
Normal levels do not rule out lead toxicity!
g) h)
ASO and DNase B antibodies Rapid Strep and throat culture with any suspicion of throat discomfort
10
i)
Quantitative Immunoglobulins (antibodies)
(1)
IgE, IgA, IgG, and IgM
j)
Quantitative IgG and IgM levels for
(1) (2) (3)
Epstein-Barr Virus (EBV) Cytomegalovirus (CMV) Herpes 6 Virus (HHV-6)
3.
Politely refuse any further vaccinations until you can consult with a Biomedical Practitioner or complete your reading.
C.
Finding a Biomedical Practitioner
1.
ARI’s Clinician List
a)
www.autism.com/dan/danusdis.htm
2. D.
Talk to parents.
Working with a Biomedical Practitioner
1.
Biomedical Practitioner as consultant
a)
You still need a Primary Medical Doctor
2. E.
Biomedical practitioner as partner
Educational therapies are as important as Biomedical therapies.
1. 2.
Hardware vs. software If your child appears ill, start Biomedical interventions first.
a) b)
A child who is sick or in pain cannot learn. Begin educational therapies as health improves.
(1)
See Appendix I
3.
If your child “appears” well, begin educational therapies first.
11
a) b)
See Appendix I Start Biomedical interventions after educational therapies firmly established.
4. III.
Maximize your child’s school experience (see Appendix J)
Protecting your affected child’s health
A.
Vaccines
1.
Risk vs Benefit
a)
Every additional vaccine given to a child on the spectrum carries a risk of further harm! Visit the National Vaccine Information Center at www.909shot.com/ Visit www.vaccination.inoz.com/ingredie.html for an examination of ingredients in vaccines. Visit www.vaccinesafety.edu/thi-table.htm for mercury content and some links to package inserts in many current vaccines.
b)
c)
d)
2.
Visit the TACA or ARI websites for alternative vaccine schedules. Read What Your Doctor May Not Tell You About Children's Vaccinations by Stephanie Cave, MD (paperback, September 2001) Visit www.fda.gov/cder/fdama/mercury300.htm for information on mercury content of other drug and biologic products.
3.
4.
B.
Dental work
1.
Amalgams (Silver colored dental fillings)
a)
>50% elemental mercury
12
b)
Give off mercury vapor which is inhaled with every breath. Still used by some dentists Should only be removed by a dentist who understands the risks of mercury exposure
(1)
c) d)
Mercury amalgam information
(a)
www.holisticmed.com/dental/amalgam/
(2)
Find a “mercury safe” dentist
(a)
www.dentalwellness4u.com
(3)
http://emporium.turnpike.net/P/PDHA/mercury/iao mt.htm for a safe amalgam removal protocol.
2.
Sealants
a)
Dental sealants are plastic resins that give off chemicals as they cure. Should only be used on permanent teeth Benefits must be weighed against risks
(1)
b) c)
Benefits
(a)
May be worthwhile in a child for whom dental cleanings require anesthesia and brushing is infrequent
(2)
Risks
(a)
Most dental sealants contain Bis-phenol A, calcium hydroxide or other toxic substances. Bacteria and food particles may eventually become entrapped under the dental sealants,
(b)
13
and can thus cause decay in the very teeth intended to be protected.
3.
Fluoride
a) b)
Evidence supporting fluoride benefits are controversial. Our kids cannot excrete excess fluoride.
C.
Being your child’s advocate
1.
Question Authority
IV.
Protecting your health and your family’s health
A.
Physical health
1.
All biological siblings of your ASD child are at risk
a)
Limit vaccines
(1)
Sane vaccine policy considers:
(a)
not vaccinating until the immune system is mature enough to handle it.
(i)
At least one year of age
(b)
not vaccinating for diseases with no significant morbidity or mortality.
(i)
Varicella (chicken pox)
(c)
not vaccinating for diseases for which the patient is not at risk.
(i)
Hepatitis B
(d)
not vaccinating early for diseases for which the patient is not at risk until much later age.
(i)
Tetanus
14
(ii) (iii) (e)
Diptheria Polio
not giving boosters until you’ve evaluated how the child responded to the initial vaccine.
(i)
Checking vaccine responses is frequently cheaper than giving boosters.
(f)
not giving combination vaccines.
(i)
Reality check: DTaP and MMR don’t exist as separate vaccines.
(g)
not giving multiple injections on the same day.
(2)
Visit the TACA or ARI websites for alternative vaccine schedules. Read What Your Doctor May Not Tell You About Children's Vaccinations by Stephanie Cave, MD (paperback, September 2001)
(3)
b)
Antibiotics only when truly necessary
(1)
Viral infections do not respond to antibiotics.
(a) (b)
60% of all ear infections are viral! The majority of all childhood bronchitis, pneumonia, sinusitis and pharyngitis (sore throat) are viral. If you visit an urgent care or emergency department, you will likely leave with an antibiotic prescription.
(c)
15
(2)
Throat infections only require an antibiotic if they are documented Group A Streptococcus. Just because a cold lasts longer than a week does not mean it requires an antibiotic. Persistence of high fevers and/or a child appearing increasingly ill are your best indicators of possible bacterial infection. Probiotics during and after any antibiotic course are a must!
(a)
(3)
(4)
(5)
S. boulardi (probiotic yeast) is particularly effective as it is not affected by standard antibiotics.
c)
Siblings and parents share many of the same nutritional deficiencies.
(1)
All of the supplements in our “beginning” list could benefit your affected child’s siblings. Keep doses lower with zinc, B vitamins and digestive enzymes unless you have a practitioner’s guidance.
(2)
2.
A diet that is good for the affected child is often beneficial for the family.
a)
Family members frequently share many of the same digestive and metabolic weaknesses as the affected child. Although not on the autism spectrum, many family members have issues that may benefit from dietary restriction.
(1) (2)
b)
Allergies Asthma
16
(3) (4) (5)
ADD/ADHD Learning disabilities Digestive issues
(a) (b) (c) (d)
Chronic constipation Gastro-esophageal reflux Chronic diarrhea Chronic abdominal pain
(6)
Various conditions of autoimmunity or altered immune function
B.
Financial health
1.
Have a plan.
a)
Therapies
(1)
Which and when
b)
Treatments
(1)
Which and when
c) d) 2.
Education Family and vacations
Make a budget.
a)
Investigate costs thoroughly and alter treatment plan accordingly.
3.
Have a Wish List.
a)
What treatments and therapies would we do if…?
4.
Apply for a grant.
17
a)
National Autism Association Grant
(1)
www.nationalautismassociation.org/pdf/helpingha ndapp09.doc
b)
Look for local Autism organizations who may also give grants for treatment.
5.
Consider a Fundraiser.
a)
Seek support of local autism organizations, charities and religious organizations. Organize and seek other parents for help.
b) C.
Emotional health
1.
Get rid of the guilt!
a)
You followed common practice or the advice of people you trusted.
2.
Pick your battles!
a)
Even if you think you’re “superparent,” you’re only human.
3.
Strive to make your partner a partner in your child’s recovery.
a)
80% of the parents of ASD kids divorce before the children reach adulthood. An “uninvolved” partner may have a variety of underlying issues.
(1)
b)
Guilt
(a) (b)
“I let the doctor give him his vaccines”. “It’s my genetics that made her this way!”
(2)
Denial
18
(a) (b) (c) (3)
“My child is not autistic” “I didn’t talk until I was five!” “His doctor doesn’t think it’s a problem!”
Feelings of neglect
(a)
“You care more about diets and therapies than you do about me.” “Will we ever get time alone, again?”
(b) (4)
Fear
(a) (b) (c)
“How am I going to pay for all of this?” “What will people think of us/our kid?” “How long does our life have to be this way?” “What does the future hold?”
(i)
(d)
“How do I plan for a future that is so uncertain?” “Will my child end up in an institution or in handcuffs?”
(ii)
c)
Making time for your partner is as important as recovering your child.
(1) (2)
Schedule “dates” for the two of you to be alone. Keep the lines of communication open.
(a)
Be willing to repeat yourself many times.
(i)
It doesn’t make as much sense to them as it does to you.
19
(ii)
We all have different rates of learning and acceptance.
(b)
Spend as much time listening as you do “teaching”. Send your partner to an autism conference.
(c) (3)
You can accomplish much more for your child and for your family as a team.
d)
Make one-on-one time for your spectrum child’s siblings.
(1)
A sibling’s perception will always be that the affected child gets most of the attention. This can be minimized by creating periods when the sibling has your undivided attention.
(2)
4.
You can’t take care of your child if you don’t take care of yourself! Recovery is possible!
a)
5.
The kids for whom one particular therapy is “the answer” are rare.
(1)
Beware of the “flavor of the week.”
b) D.
The road to recovery is a marathon, not a sprint.
Spiritual Health
1.
Establish/Develop/Maintain your connection with your denomination/religion/spiritual force.
a) b) c)
Prayer Devotion/Reading Meditation
20
d) e) 2.
Worship Community
This will probably be the most important thing you do for your child. You are not alone!
3.
21
Appendix A
Implementing a Gluten-Free and Casein-Free Diet (food ideas)
BREAKFAST Protein Choices: Nitrate Free (NF) turkey, chicken or pork sausage and bacon (e.g. Shelton’s® Turkey Patties and Turkey Breakfast Strips, NF Organic Valley® Pork Sausage, Jones® Light, Applegate® Bacon, and Canadian Bacon) NF Uncured Turkey Bologna (Shelton’s®) NF turkey roll-ups Eggs Refried Beans on a corn tortilla with or without eggs Nut butter on GF toast or waffle - can use cashew, macadamia, almond or sunflower (Sunbutter®) which is available in stores. Mail-order through www.specialfoods.com for pecan or brazil nut, etc. Carbohydrate Choices: Waffles –GF/CF-Less refined, high fiber flour choices are preferred. Pancakes - (mail-order Authentic Foods® www.authenticfoods.com has healthy bean flour. There are numerous other brands but most have less fiber.) Consider making your own. Breakfast bars (e.g.Glutino®) GFCF bread (e.g.Kinnikinnick®, Food for Life®, Energ-y®, Glutino®) Cereals (Barbara’s Brown Rice Crisps®, Erewhon Crispy Brown Rice with Berries®, GF corn flakes, Puffins Honey Rice®, Envirokidz Panda Puffs® and Gorilla Munch®, Rice Crunch-ums®, Natures Path Honey’d Corn Flakes® and Mesa Sunrise®, Nu-World Amaranth Cereal Snaps®, Perky’s Nutty Rice®, Perky’s Perky D’s) Many of these brands have high sugar content so use in moderation. Dairy-free Milk Choices: Rice Milk Almond Milk
22
Hazelnut Milk Hemp Milk Vance’s Dari-Free® (potato based) Fats and Oils: Olive oil (virgin cold pressed) Earth Balance® Margarine Ghee Coconut oil (use organic e.g. Tropical Source®) Expeller pressed oils Spectrum® shortening for frying Sugar Options: Raw honey or locally made honey Real maple syrup Molasses GF brown rice syrup Agave Stevia LUNCH Coconut yogurt (So Delicious®) GFCF bread with nut butter and jelly NF lunch meat roll-ups, GF crackers and fruit Meat “Pizza” Muffins and nuts Bean dip with veggies and chips Falafel’s with tahini on corn tortilla (falafel mix from Authentic Foods®) Chicken leg par-boiled and then fried in GF breadcrumbs. Grilled Tofutti® cheese and NF ham Leftovers from GFCF dinners DINNER Main Dishes – see the many good GFCF cookbooks available Vegetables - try roasting veggie’s with olive oil or puree and add to sauces and soups.
23
SNACKS Jennie® Coconut Macaroons Pamela’s® Cookies (check label, some are not dairy-free) Potato Chips (most brands GFCF but try to buy one with expeller pressed oil) Potato stix Popcorn (make your own) Ener-g Pretzels® with or without sesame Lungberg® Rice Chips original Robert’s American Gourmet Potato Flyers® and Veggie Booty® Dehydrated veggies and fruits (Whole Foods, Health food stores) Terra® Parsnip, Taro and Sweet Potato Chips and Terra Stix® Enjoy Life® has many varieties of cookies Envirokidz® Animal Cookies Glutino Vanilla Dreams® Midel® Choc Sandwich (like oreos) Midel® Ginger Snaps Nuts all kinds (except peanuts) - raw is best Seeds Dried fruit Rice crackers Ener-G® crackers Glutino® Breakfast Bars Organic Food Bar™ from www.organicfoodbar.com (also available at Whole Foods) Archer Farms® no dye fruit bars (available at Target)
Other foods to have on hand to use in recipes: Earth’s Best® Pear Sauce to use instead of apple sauce Earth’s Best® Sweet Potatoes and/or Acorn Squash to use in recipes Earth’s Best® Bananas for banana bread or pancakes (can use fresh also) Bearitos® Taco Seasoning or another GFCF brand Chicken broth (Pacific® or Shelton’s® Brand) Beef broth (Pacific®) GF Baking Powder (e.g. Featherweight®-use aluminum free) Brown rice flour
24
White rice flour Potato starch Tapioca flour Almond flour Coconut flour Arrowroot flour to thicken sauces Other GF flours – there are many healthy options if blended with some of the above choices. Use them when you cook or bake from scratch. Refried Black or Pinto Beans Instant Mashed Potatoes Olive Oil and Vinegar Salad Dressing Alcohol Free Vanilla Organic Coconut Milk (e.g. Thai Kitchen®, Whole Foods®) Tinkyada® pasta (different kinds) Quinoa elbow pasta Hard shell tacos and/or corn tortillas Spaghetti sauce (check ingredients, no dairy) Barbecue Sauce (e.g. Saz’s®) Cascadian Farms® French Fries Salt – a good brand is essential (Himalayan or sea salt)
GFCF “Packaged Foods” See www.gfcfdiet.com shopping guide for many brand names. Chili (check ingredients) Thai Kitchen® Meals (check ingredients) Shelton’s® Chicken and Rice soup GFCF Spaghetti O’s Gerber Graduates® Chicken and Rice Ian’s® Chicken Nuggets or Turkey Corn Dogs Welshire Kids® Chicken Bites or Bell and Evans® GF Chicken Nuggets and other chicken products Saz’s® shredded chicken in barbecue sauce Useful kitchen appliances and gadgets: Toaster oven Deep fryer Cast iron frying pan
25
French fry maker Smoothie machine Food processor Grater Garlic press
The brand names listed here are those that in our experience have proved useful. They are intended as a guide for parents who are new to healing diets and the list is by no means exclusive or exhaustive. There are many other good brands, and many that vary from region to region. Also, many companies change ingredients without notifying consumers and so it is always prudent to read labels and contact manufacturers to confirm ingredients at the time of purchase.
26
Appendix B
Everything You Didn’t Want in Your Child’s Food
All aluminum compounds Artificial colors Artificial flavors Aspartame (Nutrasweet®) BHA BHT Caffeine F D & C colors Monosodium Glutamate (MSG) AKA Modified food starch Hydrolyzed soy protein Hydrolyzed yeast protein Nitrates Nitrites Phosphoric acid Potassium Bromate Quinine Olestra Polysorbate 60, 80 Saccharin Sucralose (Splenda®) Sulfites Vanillin (common artificial flavor) TBHQ
27
Appendix C
Basic Supplements for Autism Treatment
Probiotics: Probiotics are beneficial bacteria given to help re-populate and rebalance the normal intestinal flora. Levels of these beneficial bacteria are frequently low or absent due to antibiotic use, gastrointestinal inflammation, and low immune function. Benefits of probiotics can include control of yeast (Candida), parasites, pathogenic (bad) bacteria, and viruses. Additional benefits can be improved digestion and absorption and resolution of abdominal pain. While certain strains of probiotics can be used to target specific problems, a general or multi-strain probiotic formula is needed to provide basic support. It is generally a good idea to start with a basic probiotic with a strength of about 10–15 billion organisms per capsule and to begin dosing with ½ capsule and increase as tolerated. Quality probiotics typically require refrigeration to maintain potency. Some good brands for general multi-strain probiotics include Floragen®, Klaire Ther-biotic Complete®, Theralac® and Kirkman Pro-Bio®. Usually probiotics are better absorbed on an empty stomach. Give probiotics 30 minutes before or at least 2-3 hours after eating. Probiotic supplements that can be used to target specific problems: Culturelle® (does not require refrigeration) – can be beneficial for yeast (Candida) and Clostridia overgrowth, and also for management of urinary tract infections. Threelac® - can be beneficial for yeast problems. VSL #3® – use this brand if there are oxalate issues. Magnesium: Magnesium is another mineral necessary for many enzymatic processes within the body and is calming for the neurologic system.
28
Available forms include magnesium citrate, magnesium glycinate, magnesium oxide and magnesium malate. Magnesium citrate is the desired form when constipation is a problem. Dosage can be adjusted as needed to produce desired stool consistency for alleviation of constipation. Magnesium glycinate and magnesium oxide are used for better absorption when constipation is not an issue or if a person has diarrhea. Dosage is typically fixed and can be adjusted to obtain desired serum or erythrocyte (red blood cell) levels. Magnesium malate can be beneficial in helping to control seizures in some seizure disorders. Typical doses of all forms are 120 – 200mg of elemental magnesium once to twice a day. Zinc: Zinc is necessary for multiple enzyme processes in the body. Available forms include zinc citrate, zinc picolinate and zinc sulfate. A combination of these may be necessary to obtain desired serum zinc levels. Some improvements seen in our practice from zinc supplementation include improved sensory processing, improved taste and appetite, and improved sleep. Dosing could start at 15-30mg per day. Do not give zinc with digestive enzymes. Vitamin C: Vitamin C is a powerful anti-oxidant and anti-viral agent. As a watersoluble vitamin, it can also be beneficial in alleviation of constipation. For anti-viral and anti-oxidant support, dosage is typically fixed and increased in increments if being well tolerated. It is important to get a buffered brand to reduce GI upset. For constipation, dosage is usually titrated (dosage goes up or down based on symptoms) according to stool consistency. Dosages can range from 500mg up to 4,000mg or more. Suggested brands include Longevity Plus Bio En’R-G’y C® (good absorbability – better for anti-viral and anti-oxidant support), Perque® Potent C Guard, Allergy Research Group®, and Pure Encapsulations®. If there is an oxalate issue, it is not recommended to supplement Vitamin C at greater than 500 mg/day.
29
Essential Fatty Acids: Essential fatty acids can be beneficial for neurological healing (repair of myelin) and can also function as an anti-inflammatory agent. Sources include cod liver oil, fish oil, and supplements containing DHA and EPA, EPO and Flax. If a strong aversion to the fish oil exists, the essential fatty acids can be obtained in a pudding form from such brands as Coromega®, and Springboard®. Due to mercury contamination of fish, a reputable company that purifies and removes contaminants such as mercury must be used. Nordic Naturals®, Kirkman®, Coromega® and Carlson’s® are some reputable companies that make quality products. There are other good brands, so be sure to check ingredients and fish source, and make sure the company will put in writing that their products are free of heavy metals.
Multivitamin: A good multivitamin can provide necessary nutrients that can be lacking due to malabsorption, increased metabolic demands, restricted food choices, and decreased nutrient quality of over processed or poorly grown foods. Multivitamin sources should be free of iron and copper as these can increase oxidative stress and require metabolism through the same process necessary for detoxification of heavy metals. Individual supplementation of iron or copper may be indicated based on lab results. Many forms of multivitamins exist from liquid to chewables, gummies, or capsules. Suggested brands include Nordic Naturals®, Animal Parade®, and Rhino Vites® for gummies; Springboard® and Kirkman® for chewables; Biotics Research®, Brainchild®, and Kirkman® for liquid forms; and Child Essence® and Kirkman® for capsules. Targeted Nutritional Therapy: There are many other supplements that are used to drive metabolic processes. These include oral B vitamins and methyl B shots. Types and doses are prescribed on an individual basis. DMG, TMG and high dose B vitamins should be given earlier in the day as they may cause increased hyperactivity and stimming. Doses may need to be adjusted until the child gets used to them.
30
Appendix D
Dosing Guidelines for Constipation Treatment Magnesium Citrate and Vitamin C
Magnesium Citrate – Begin with 100 – 150 mg daily. Increase dose every 2-3 days up to 400mg twice a day. Vitamin C (buffered) – It is important to use a buffered formula when using higher doses. Vitamin C is ascorbic acid and may cause GI upset if a buffered formula is not used. Begin with 250 mg/day dose. If not effective, increase the dose every 2-3 days up to 2000 mg twice a day. The goal is 2-3 bowel movements (BMs) daily that are of oatmeal consistency. Begin with magnesium citrate, then, add in Vitamin Calternately increasing the dose of each until BMs are of a desired consistency. If diarrhea develops, back off the dose of one or both if needed. If constipation remains a problem and you are at the highest dose of both Vitamin C and Magnesium, consider adding Oxy-Powder® up to 2 capsules twice a day.
31
Appendix E
Probiotics
Probiotics are the GI tract’s “good bacteria” that help to strengthen our immune system and aid in food digestion. Many times, frequent courses of antibiotics can kill off a body’s good bacteria, which can weaken the body’s immune system and allow bad bacteria and fungi (yeast) to grow and flourish. Probiotics can help rebalance the GI tract, boost the immune system, and kill off yeast. At least 75% of our body’s immune system lies in our GI tract. Probiotics need to be given on an empty stomach. When food is given with probiotics, the stomach acid that is produced with food can interfere with the probiotics and will not allow the probiotics to work as well as they should. The general rule for probiotics is 20 minutes before food or 2 hours after food. The most common times to give probiotics are right away in the morning and at night before bed. Try to give the morning probiotics dose before breakfast in a drink or syringe for an oral dose. If able to swallow pills, take probiotics with a half glass of water. Start with half of a capsule of the recommended probiotics in the morning. Watch your child for any negative behaviors which might be yeast die-off. If your child has any negative behaviors, back down to ¼ capsule in the morning and watch your child again. If your child is tolerating the initial dose (¼ or ½ of a capsule) in the morning, then add ½ of a capsule in the evening before bed, remembering the rule of two hours after food. If your child can tolerate the ½ capsule in the morning and evening, then increase to a full capsule in the morning and a ½ capsule at night. Again, watch your child for any negative behaviors. A common complaint of beginning probiotics is bad behavior, aggression, increased stimming, and worsening of bowel movements (either diarrhea or constipation). These are all symptoms of yeast die-off.
32
If you think your child is tolerating the 1 full capsule in the morning and ½ capsule in the evening, then increase the dose to 1 full capsule in the morning, and 1 full capsule in the evening, which is the optimal dose. Hold at that dose until your next appointment when Dr. Brown will determine if the dose should be increased or the probiotics should be changed to a different type. Probiotics come in different strengths (counted by millions or billions of bacteria or cfu) and strains (3, 5, 8, etc.) The general rule is to keep going higher, working within the tolerance of your child. If using the probiotic VSL (prescription), start at 1/16 or 1/8 tsp daily. If tolerating, increase dose to twice daily. Gradually increase each dose as tolerated until at recommended dose (typically ¼-½ packet twice daily). Please note that it may take anywhere from a few weeks to several months to reach this dose.
33
Appendix F
Activated Charcoal for Yeast Die-off
Yeast imbeds itself into the GI tract and lines the GI tract with little toxic pockets. These little yeast pockets cause damage when they live in the GI tract. However, when the toxic pockets are being killed off with anti-fungal medications, these pockets burst, and cause intense pain in the GI tract, or even other places in the body, depending on the type and severity of the yeast problem. Just to give you an idea of how severe the pain can be, many people, adults included, cannot complete yeast treatment because the pain is so severe. This extreme die-off is called the Herxheimer reaction. Activated Charcoal is generally used to absorb toxins from the GI tract. In high doses, Activated Charcoal has been safely used in cases of poisoning, overdoses, etc. Activated Charcoal can safely escort the toxins caused by yeast out by encapsulating them and preventing the toxins from causing intense pain on their way out of the body. Activated Charcoal comes in a capsule form. It is a much lower dose than the doses used for poisoning. If your child can swallow pills, it will be easier for your child to take Activated Charcoal. But if your child does not swallow pills, the contents of the opened capsule can be put into water, or given on a spoon in a dark substance such as raspberry sorbet or a crushed up GFCF Oreo like a Mi-Del or a K-Too. The black powder inside the capsule is gritty, but doesn’t really have any taste. An opaque cup with a sport top or white athletic water bottle works well because the charcoal will turn the water black. Some brands are less gritty than others, ask your clinician for brand suggestions. There are several rules to follow when administering Activated Charcoal. Activated Charcoal will absorb EVERYTHING in the stomach, even nutrients, medications, and supplements. The general rule is to give Activated Charcoal 1½ to 2 hours after food, meds, and supplements. The best way to do this, is to give the anti-fungal medication with a meal, trying to make sure the child eats as much as possible at the meal so the child is not hungry later, like when it is time for the child to get the Activated Charcoal in 1½ to 2 hours. The Activated Charcoal also has to be given 1½ to 2 hours
34
BEFORE eating the next meal. You need a 4 hour window between meals when using Activated Charcoal. It can tricky to make sure the child is eating enough at meals during yeast die-off because appetite changes can occur at this time. During yeast die-off, taste can also change temporarily. Favorite foods may be refused and/or the child may limit themselves to just one or two foods, especially carbs. The die-off should lessen and over time, the Activated Charcoal won’t be necessary at all. Your child may only need Activated Charcoal when the dose of anti-fungal medication has been increased. Dosing for Activated Charcoal is according to weight. A general rule is: under 50 lbs- ½ to 1 capsule 2-3 times daily and over 50 lbs- 2 capsules 2-3 times daily. Activated Charcoal can cause constipation. If this occurs, try another similar product called Citrus Pectin. It is trial and error to see which of these two will be tolerated best by an individual child. Dosing for Pectin: Under 50 lbs, ½ of a capsule. Over 50 lbs, 1 full capsule.
35
Appendix G
Supplement Dosing Techniques
Supplements can be quite a challenge to give to a child with sensory and language issues. If your child is unable to swallow pills there are two basic approaches: hide it in something or just be upfront and give it by mouth with a syringe. If you think your child will do better with hidden supplements, some ideas are to crush tablets or open capsules and mix in juice, applesauce, peanut butter, or any other food you think will work. Sippy cups and sport bottles work great because you can’t see the liquid inside and some supplements may change the color or leave a little residue on top of the liquid. This change is enough to make some kids refuse to even try it. Another good trick is to start with small amounts and gradually increase the amount to allow your child’s taste to adapt. Another technique is to be upfront with your child and use a syringe (without a needle) to give the supplements. If your child is refusing to eat certain foods, suspicious they may contain supplements, this technique may work best for you. First, give your child a mouthful of plain water with the syringe. Then let them play with the syringe in a cup of water. This helps them to realize the syringe will not hurt them. You can reverse these steps if you like. The first time, someone may need to hold your child to help you get the water in their mouth. The next step is to give your child some juice with the syringe. Do this a few times to help them get used to it. Now you are ready to start adding in supplements. Start with very small amounts and gradually increase the amount as your child’s taste adapts. Some supplements taste better than others, so you may need to taste them to know which ones you will need to dilute more and which ones can be more concentrated. If your child has been through some ABA, then they know about reinforcement. It can be very helpful to reward them with a small treat once they swallow (food, computer time, etc) If you use food as a reward please try to keep it relatively healthy and keep in consideration your child’s own unique biomedical needs and issues.
36
Additional tips that have worked for some parents: No “free” undiluted juice! Always, always, always have a supplement or medication in a full strength juice. Start by becoming a mixologist for your child and mixing a juice that has one consistent taste throughout the day. By the time you add all their supplements and find the right juice combination to mask the taste, the juice that you end up with will not resemble anything that you started with. That doesn’t mean it won’t be flavorful enough for your child to drink. Generally, all the juice can be made right away in the morning and refrigerated or sent to school, day care, etc. Write down what you are adding to the juice so that you can get your “formula” down and be consistent with your child’s juice. Any other juice your child drinks should be diluted to at least 50% with water. Juices that are recommended are White Grape Juice and Pear juice because they are low in salicylates. Santa Cruz makes an organic White Grape Juice in a glass bottle. Welch’s makes a White Grape juice concentrate in the frozen section that is 100% juice. Juice concentrate from the can: Pour an entire can of concentrate into a container to store in your refrigerator. Use 1 teaspoon of concentrate for anywhere from 2 to 6 oz of water as needed. The concentrate can be helpful for particularly bitter medicines where the regular strength juice is not enough. GF/CF sorbets and frozen desserts can hide many supplements in a relatively small volume. These are just a few tips. If supplement dosing continues to be a problem, contact your biomedical practitioner or ask some other parents how they give them to their children. Parents who are dedicated to helping their children can be very creative and resourceful when challenges arise. GOOD LUCK!
37
Appendix H
Everything You Didn’t Want to Know About YEAST And Were Afraid to Ask
Yeast is one of the most significant and serious health issues facing children on the autism spectrum. The primary species of yeast that affects our kids is candida albicans. Yeast is a chronic condition and may need to be treated repeatedly. Yeast can impact many different parts of the body, but can significantly affect the GI tract. Yeast creates little pockets filled with toxins that imbed themselves in warm, moist places. The lining of the GI tract is a perfect place for yeast to live and set up housekeeping. Lab tests are available to test for yeast, but the tests are frequently unreliable, that is there can be many false negatives. A negative test does not rule out a yeast problem. The diagnosis can be helped by testing the blood, urine or stool but frequently clinical exam and patient history are most reliable. Sometimes, the only way to know if a child has an overwhelming yeast problem is to treat for yeast and look for yeast die-off. Symptoms of yeast overgrowth/flare ups can include: headaches, even migraines, stimming, hyperactivity, severe abdominal pain, cravings for sugar and carbs, aggression associated with pain, joint pain, fatigue, and pain in strange areas of your child’s body: feet, genitals. A common symptom of yeast is excess giggling and laughing. Giggling and laughing in the middle of the night is very common and can wake some children out of a deep sleep for a few hours at 3:00am, or some other inappropriate time. Some children will go back to sleep for a few hours, some will not. This disturbed sleep pattern can go on for a prolonged period, even years. When yeast has had longer to infiltrate the body, behaviors can be worse than excess giggling and laughing. Often times, the pain becomes unbearable for ASD children with yeast, especially as the child ages. The yeast multiplies and imbeds itself further, causing more pain and damage internally. One of the biggest problems is that children on the spectrum cannot tell where it hurts or the severity of the pain. The child’s only way to communicate is to act aggressively with a pinch, bite, or slap. The intense pain the child feels and the resulting aggression can be similar to labor contractions. Women sometimes find it helpful to squeeze another person hand during labor. ASD children will sometimes get relief with an
38
aggressive pinch or bite. This aggression can be misunderstood to be a behavioral issue, like a tantrum. Many children have had their “behavioral issues” reduced significantly with anti-fungal medications when the child’s pain resolves. Candida albicans have a short life-span therefore anything that feeds them also causes more of them to be dying and the chemicals that cause our kids problems are released when they die. When we do things that are intended to kill off yeast (probiotics, natural or pharmaceutical antifungals), we should expect what we refer to as “yeast die-off”. Yeast die-off looks different in every child and the only way to truly know when your child is having a yeast flare up/overgrowth or die-off is by observation. As stated above, the excess giggling can be a symptom of yeast flare up, usually an early stage yeast infiltration. Pain and crying that seems to escalate as time goes on can be later stage yeast growth. When treated with anti-fungal medication, the pain should lessen considerably and the child should begin to have pain only after a dose of anti-fungal medication. Yeast treatment can take several months, and complete containment of yeast issues can take years, but treatment often significantly helps the ASD child. Warning about antibiotics: If a child is identified as having a chronic yeast problem, the child needs to be back on some aggressive form of yeast treatment during and after the course of antibiotics. Yeast is a chronic condition and can re-emerge at any time.
39
Appendix I
Non-medical Treatment Options for Autism Spectrum Disorders
A Home Program consisting of at least 25 hours of 1:1 therapy is the core of educational treatment for autism. Please see the book put out by the National Research Council, Educating Children with Autism. The book explains the need for 1:1 therapy ALL YEAR LONG. This may be helpful in IEP (Individualized Educational Program) meetings because it contains research and guidelines put out by our government. Therapy can consist of one or more of the core educational programs listed below. Methodology can be individualized for each child, however, some feel that ABA has the most research behind it. The decision should be made by the parents after investigating all options. ABA - Lovaas®, Verbal Behavior®, DTT (Discrete Trial Training) are examples of ABA Books and resources: Behavioral Intervention for Young Children with Autism by Catherine Maurice Various books, websites and workshops by Dr. Vince Carbone or books and information by Mark L. Sundberg, PhD and James W. Partington, PhD DIR®/FloorTime™ - Dr. Greenspan recommends relationship-based play therapy. Books and resources: Engaging Autism: Using the Floortime Approach to Help Children Relate, Communicate, and Think by Serena Wieder and Stanley Greenspan The Affect-Based Language Curriculum (ABLC) by Greenspan and Diane Lewis www.icdl.com RDI® - Relationship Development Intervention Books and resources: www.rdiconnect.com Autism Aspergers: Solving the Relationship Puzzle by Steven Gutstein, PhD
40
Relationship Development Intervention with Young Children: Social and Emotional Development Activities … by Steven Gutstein, PhD and Rachelle Sheely The above programs are considered core educational programs. Additional interventions may be added at different times depending on individual symptoms. Each intervention should address specific deficits. It is often necessary to treat autism with multiple interventions on the road to recovery. Of course, speech therapy, OT (occupational therapy) and sometimes PT (physical therapy) are essential in addition to the above core home program(s), and ideally the therapists should work together to integrate and generalize skills. In the early years, it is most beneficial for your child to do neurotypical preschool with an aide instead of early childhood special education programs, in order to optimize peer modeling. Individual situations, however, may warrant more restrictive settings. The following is an overview of different therapy options to add after the core educational program is in place. There is so much out there, however, that this list is far from exhaustive. Vision Therapy - to address deficits in visual processing skills Books and resources: Thinking Goes to School by Harry Wachs www.optometrists.org Neurofeedback – brain training www.eegspectrum.com AIT – There are many different types of Auditory Integration Training. Some web sites to search include: www.berard-ait.com Official Berard Site www.tomatis-group.com Official Tomatis Site www.integratedlistening.com Tomatis-based Training www.rmlearning.com The Listening Program (Tomatis-based) Soma®RPM - Rapid Prompting Method – focused on teaching the child using grade level curriculum leading toward independent communication. This method is especially helpful for nonverbal people and auditory learners but helps all learners. www.halo-soma.org
41
TheraPlay® - is a structured (uses intrusion) play therapy for children and their parents. The goal is to enhance attachment, self-esteem, trust in others and joyful engagement. This program is great for younger kids and serves as a short term treatment approach in conjunction with, or to get kids ready for other therapy methods. www.theraplay.org Interactive Metronome® - a program that teaches timing (and rhythm, but timing is the goal). Children will need to follow directions to comply with this program. www.interactivemetronome.com HANDLE® - Holistic Approach to Neuro Development and Learning Efficiency - a program that helps brain integration through a series of exercises prescribed by a HANDLE® practitioner. www.handle.org The Fabric of Autism by Judith Bluestone
General Educational Websites www.starfall.com www.ABCteach.com www.tlsbooks.com
Additional Reading: Reflexes, Learning and Behavior: A Window Into the Child’s Mind by Sally Goddard
42
Appendix J
Helping Parents Navigate the Educational Swamp
• Educate the teachers and staff working with your child through a “nuts and bolts” meeting. This usually is an in-service day before the kids start school. It would only last for a half hour or less but this is where you tell them about your child, medical issues, diet, etc. This is usually scheduled through the special education teacher but the principal is there as well. Keep it as short and concise as possible with handouts about your child and his/her needs. We recommend starting and ending the meeting with praise and gratitude for what they do to help your child and your family. • Communication is critical. If you don’t have a good communication system set up, just think of the most important things you want to do. Then, put it in a form the school can use and modify as necessary. It can be a check sheet or something without a lot of work for the school staff, but that gives you the information you need. For example, a tracking place for self-stims (TV talk and hand biting) and a place for bathroom use. It might also have a place for the assistants to fill in what happened in each class. The same basic concept with adaptations could be used from kindergarten through high school. E-mailing works well but is not the only option. It is important to keep the communication flowing both ways. • Be an active part of your child’s team which includes the IEP (Individualized Educational Program). Get a draft copy a few days ahead so you can read it and highlight things you want to address. This also makes the IEP move more smoothly for everyone involved. A great resource for IEP goals and objectives is www.wrightslaw.com. Again, keep in mind the most important things you want for your child’s IEP. • Make sure you document all phone calls, e-mails and other communications. This is particularly important if you think you may have difficulties, or if you have concerns about your child and his/her needs being met. After you speak with a teacher or district person,
43
write a short synopsis and mail it to the person, confirming what was discussed. E-mails can easily be deleted or never received. This strategy will help you have a paper trail, if you need to move up the district “ladder” to get the help your child needs. • Please remember that many teachers want to help your child succeed. A lot of times they have a big case load and don’t have time to follow up, etc. They may need more education about autism and strategies to help your child be more successful. You need to try and help them as best you can. • What kind of visuals are being used to help your child be successful? There are so many different kinds of visuals that can be used: visual schedules, cue cards, etc. Social stories can also be very helpful for your child to understand what will be happening. • You are your child’s best advocate. It is hard to do everything we need for our kids, but working with the school and educating them about your child will help everyone be more successful. Other places to get resources: • • • www.wrightslaw.com www.usevisualstrategies.com www.bridges4kids.org/IEP/iep.goal.bank.pdf
44
Appendix K
How to Reintroduce Casein When the GI Tract is Healed
Month 1 Try raw goat yogurt. It has smaller molecules than cow’s yogurt and because it is raw, it has naturally occurring enzymes to aid in digestion. If this is tolerated, you can also try goat butter. There is a source for raw goat milk and raw goat butter with pickup locations in the Chicago area or you may have it delivered to your home. www.belleslunchbox.com Month 2 If the raw goat yogurt is tolerated for a month, try the goat yogurt and goat cheese sold in health food stores. (Redwood Hill Farm is a good brand.) Month 3 If this is tolerated, try adding goat cheese from your local grocery store. Month 4 If everything mentioned above is tolerated, try adding cow yogurt and butter. If this is tolerated, you may try parmesan reggiano or farmer’s cheese. People with yeast problems may not tolerate aged cheeses like parmesan but may tolerate farmer’s cheese. Hard aged cheese may be easier to digest for those with dairy intolerance. Do not try any creamy cheeses or cottage cheeses. If possible, it is best to stay with raw milk. (www.realmilk.com) Also, any fermented foods that are added to the diet can prevent and heal leaky gut because they add natural probiotics. Read The Untold Story of Milk, by Ron Schmid ND and Nourishing Traditions by Sally Fallon for more information.
Note: The reintroduction of gluten and casein should be at least 2 months apart from each other. Wait until one is completely introduced before trying to add the other. If
45
trying to reintroduce both gluten and casein, start with casein because the reactions to gluten may be delayed and may take weeks or months to build up and cause symptoms.
46
Appendix L
How to Reintroduce Gluten When the GI Tract is Healed
Month 1 Try McCann’s Steel cut Irish oats. Month 2 If tolerated, try barley in soups, flours, or cereal. Month 3 If oats and barley are tolerated, you can try rye. This could be difficult since most products made with rye also have wheat in them. There are all rye crackers and you may find all rye bread at specialty stores. Introducing rye at this point, however, is optional. Month 4 If oats, barley, and rye are tolerated, try bread made with sprouted wheat. An example is Ezekiel bread. Month 5 If above mentioned grains are tolerated, you can add products made with whole wheat. (Note: there is no difference between products made from white flour or whole wheat flour, either from an allergy perspective or peptide perspective. In fact, some whole wheat products may have more gluten. Of course, white flour is bad for everyone, because it has very little nutrition and a high glycemic index which means it feeds yeast and other bad gut bugs.) Month 6 If everything mentioned is tolerated, patient can occasionally have a special treat of white bread. For example, pizza out with the family might be ok. In most cases, white bread should be avoided because of its lack of nutrition.
Note: The reintroduction of gluten and casein should be at least 2 months apart from each other. Wait until one is completely introduced before trying to add the other. If
47
trying to reintroduce both gluten and casein, start with casein because the reactions to gluten may be delayed and may take weeks or months to build up and cause symptoms. If wheat is reintroduced and symptoms reoccur months later, then a person may not tolerate wheat on a daily basis. The recommendation, then, would be to remove gluten until all symptoms are gone and then try to eat it on a rotation (every 4-7 days) basis. Continue only if symptoms do not reappear.
48
Appendix M
Autism Book List
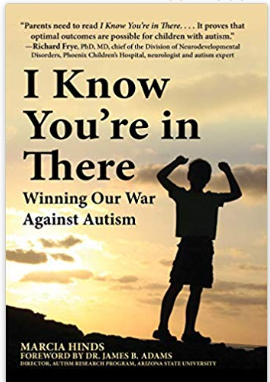
Cookbooks/Dietary
Special Diets for Special Kids I & II by Lisa Lewis, PhD Breaking the Vicious Cycle by Elaine Gottschall Nutrition in a Nutshell--Build Health & Slow Down the Aging Process by Bonnie C Minsky, M.A., MPH, CNS, LNC Special Diet Celebrations by Carol Fenster, PhD The Candida Albicans Yeast-Free Cookbook by Pat Connolly The Feingold Cookbook for Hyperactive Children by Ben F. Feingold, M.D. and Helene S. Feingold Enzymes for Autism and Other Neurological Conditions by Karen DeFelice Smart Fats by Michael A Schmidt Feast Without Yeast by Bruce Semon MD, PhD and Lori Kornblum Cooking Healthy Gluten and Casein Free Food for Children by Betsy Prohaska 200 Flavorful Recipes for People with Food Allergies and Multiple Food Sensitivities by Carol Fenster, PhD Gluten-Free Diet: A Comprehensive Resource Guide by Shelley Case, B.Sc.H.Ec., P.Dt., Registered Professional Dietitian The Body Ecology Diet: Recovering Your Health and Rebuilding Your Immunity by Donna Gates and Linda Schatz Nourishing Hope, Nutrition Intervention for Autism Spectrum Disorders by Julie Matthews The Kid-Friendly ADHD & Autism Cookbook by Pamela J. Compart, MD and Dana Laake, R.D.H.,M.S., L.D.N.
Stories Louder than Words by Jenny McCarthy Unraveling the Mystery of Autism and Other Pervasive Developmental Disorder by Karyn Seroussi Overcoming Autism by Lynn Kern Koegel, PhD
49
Facing Autism by Lynn Hamilton & Bernard Rimland Nobody Nowhere, Somebody Somewhere by Donna Williams News from the Border by Jane Taylor McDonnell Autism: Heartfelt Thoughts from Mothers by Judy Lynne
General Healing and Preventing Autism: A Complete Guide by Jenny McCarthy and Jerry Kartzinel M.D. Ten Things Every Child with Autism Wishes You Knew by Ellen Notbohm Ten Things Your Student Wishes You Knew by Ellen Notbohm Thinking in Pictures by Temple Grandin Emergence: Labeled Autistic by Temple Grandin The Out of Sync Child by Carol Kranowitz Is This Your Child? by Doris Rapp
Vaccines What Your Doctor May Not Tell You about Children's Vaccinations by Stephanie Cave MD Vaccines, Autism and Childhood Disorders by Neil Z. Miller Evidence of Harm by David Kirby
Biomedical Autism: Effective Biomedical Treatments by Jon Pangborn, PhD & Sidney MacDonald Baker, MD Children with Starving Brains by Jaquelyn McCandless, MD Healing the New Childhood Epidemics : Autism, ADHD, Asthma and Allergies by Kenneth Bock, MD Changing the Course of Autism by Bryan Jepson, MD Recovering Autistic Children by Stephen M Edelson, PhD & Bernard Rimland, PhD Hyperbaric Oxygen Therapy by Richard Neubauer, MD & Morton Walker, DPM Genetic Bypass Using Nutrition to Bypass Genetic Mutations by Amy Yasko, MD
50
Therapies Relationship Development Intervention with Young Children by Steven E Gutstein & Rachelle Sheely The Fabric of Autism (HANDLE) by Judith Bluestone
Dietary Websites and Mail Order Foods www.namaste.com www.glutenfreemall.com www.glutenfree.com www.glutensolutions.com www.kinnickinnick.com www.pamelasproducts.com www.gfcfdiet.com www.authenticfoods.com www.specialfoods.com
Other Websites www.enzymestuff.com
The following individuals have contributed selflessly to this effort Vicki Martin RN Jane Sparks RN Deanna Davis RN Stephanie Mauck Becky Accetta Katie Hansen Rev. Kathy Brown
51